Assisted living facility regulations are the cornerstone of ensuring safe, high-quality care for seniors who need assistance with daily living activities. These regulations, which vary by state, encompass a wide range of topics, from licensing and certification requirements to resident rights and staff qualifications.
Navigating this complex landscape is crucial for both residents and their families, as well as for facility operators who must ensure compliance. This guide will provide a comprehensive overview of assisted living facility regulations, highlighting key aspects and addressing common questions.
Overview of Assisted Living Facility Regulations
Assisted living facilities (ALFs) provide housing and supportive services for individuals who need help with daily activities but do not require the level of care provided by a nursing home. Regulations governing ALFs are designed to ensure the safety, health, and well-being of residents, while also promoting quality care and ethical practices.
Also Read
Navigating the complex regulatory landscape of assisted living facilities requires a deep understanding of local and state laws. From licensing requirements to resident care standards, the legal framework can be daunting. Seeking expert guidance from legal professionals, such as those specializing in Business Formation Legal Advice Navigating the Legal Landscape , can ensure compliance and mitigate potential risks. This comprehensive legal support can help operators avoid costly penalties and maintain a safe and ethical environment for residents.
Purpose and Scope of Assisted Living Facility Regulations
Assisted living facility regulations aim to establish minimum standards for the operation of ALFs, covering various aspects, including resident rights, staffing requirements, physical plant standards, emergency preparedness, and resident care. These regulations are intended to:
- Protect the health, safety, and welfare of residents.
- Ensure that residents receive appropriate care and services.
- Promote a safe and comfortable living environment.
- Provide transparency and accountability in the operation of ALFs.
Historical Development of Assisted Living Facility Regulations
The development of ALF regulations has been influenced by a number of factors, including:
- The growing number of older adults in the population.
- The increasing demand for alternative care settings to nursing homes.
- The recognition of the need for specialized care for individuals with cognitive impairments.
In the 1980s, the first ALF regulations were established in several states, and the number of states with ALF regulations has continued to grow since then.
Key Federal and State Agencies Involved in Setting Regulations
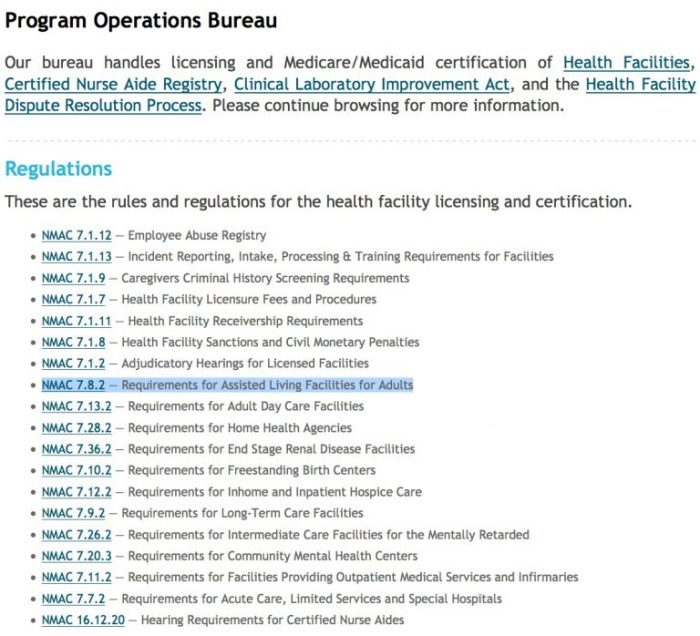
At the federal level, the Centers for Medicare & Medicaid Services (CMS) plays a role in regulating ALFs through the Medicare and Medicaid programs. CMS sets standards for the quality of care provided by ALFs that participate in these programs.
- The Centers for Medicare & Medicaid Services (CMS)
- The Department of Health and Human Services (HHS)
State governments also play a significant role in regulating ALFs. State agencies responsible for regulating ALFs typically have the following functions:
- Licensing and certification of ALFs.
- Enforcement of state regulations.
- Investigation of complaints.
- Education and training for ALF staff.
Licensing and Certification Requirements
Assisted living facilities (ALFs) are subject to specific licensing and certification requirements, which vary by state and jurisdiction. These requirements ensure that ALFs meet minimum standards for safety, quality of care, and resident well-being.
The process for obtaining and maintaining these licenses and certifications involves several steps, including application, inspection, and ongoing monitoring. The criteria used to evaluate compliance with licensing standards are based on a range of factors, including facility infrastructure, staffing levels, resident care plans, and emergency preparedness.
Licensing Requirements
Most states require assisted living facilities to obtain a license to operate. The licensing process typically involves the following steps:
- Application: Facilities must submit an application to the state licensing agency, providing detailed information about the facility, its services, and its staff. This application may include information about the facility’s physical layout, staffing ratios, resident care plans, and emergency procedures.
- Inspection: Once the application is reviewed, the state licensing agency will conduct an inspection of the facility to ensure it meets the minimum standards for safety, quality of care, and resident well-being. This inspection may include a review of the facility’s physical environment, its staffing levels, and its resident care plans.
- License Issuance: If the facility meets the licensing requirements, the state licensing agency will issue a license to operate. The license is typically valid for a specified period, and the facility must renew it periodically.
Certification Requirements
In addition to licensing, some states require assisted living facilities to obtain certification from a federal or state agency. Certification may be required for facilities that participate in certain government programs, such as Medicaid or Medicare.
- Medicare Certification: Facilities that participate in Medicare must meet specific standards for quality of care and safety. This certification process involves a rigorous inspection and review of the facility’s operations.
- Medicaid Certification: Facilities that participate in Medicaid must also meet specific standards for quality of care and safety. The certification process for Medicaid is similar to that for Medicare.
Compliance Evaluation Criteria
State licensing agencies use a variety of criteria to evaluate compliance with licensing standards. These criteria may include:
- Physical Environment: The facility must meet certain standards for safety and accessibility, including adequate lighting, ventilation, and fire safety measures.
- Staffing Levels: The facility must have sufficient staff to provide adequate care to residents. This may include registered nurses, certified nursing assistants, and other licensed professionals.
- Resident Care Plans: The facility must develop individualized care plans for each resident, addressing their specific needs and preferences. These plans should be reviewed and updated regularly.
- Emergency Preparedness: The facility must have a plan in place to address emergencies, such as fire, power outages, or natural disasters. This plan should include procedures for evacuating residents, contacting emergency services, and providing care to residents in the event of an emergency.
- Resident Rights: The facility must respect the rights of residents, including their right to privacy, autonomy, and dignity. Residents should be informed of their rights and have access to grievance procedures.
Resident Rights and Protections
Residents of assisted living facilities have fundamental rights and protections that ensure their well-being, autonomy, and quality of life. These rights are enshrined in federal and state laws, as well as in the facility’s own policies and procedures.
Privacy Rights
Residents have a right to privacy in their personal lives, including their living spaces, communications, and medical information. This means that residents can expect a certain level of confidentiality and respect for their personal boundaries.
- Private conversations: Residents have the right to engage in private conversations without being overheard or monitored by staff or other residents.
- Personal belongings: Residents have the right to keep their personal belongings in their living space and to control who has access to them.
- Medical records: Residents have the right to access their own medical records and to control who can see them.
Autonomy and Decision-Making
Residents have the right to make their own decisions about their care and living arrangements. This includes the right to choose their own doctor, to refuse treatment, and to participate in decisions about their care plan.
- Choice of care: Residents have the right to choose the type and level of care they receive, as long as it is consistent with the facility’s capabilities and the resident’s needs.
- Refusal of treatment: Residents have the right to refuse any treatment, including medication, even if it is recommended by their doctor.
- Living arrangements: Residents have the right to choose their living arrangements, such as their room or apartment, and to personalize their space with their own belongings.
Safety and Security
Residents have the right to live in a safe and secure environment. This means that the facility must take steps to protect residents from harm, including physical abuse, neglect, and exploitation.
- Physical safety: The facility must provide a safe environment for residents, including measures to prevent falls, fires, and other accidents.
- Abuse prevention: The facility must have policies and procedures in place to prevent and respond to abuse, neglect, and exploitation of residents.
- Emergency preparedness: The facility must have a plan in place to respond to emergencies, such as fires, floods, or power outages.
Resident Advocacy Groups
Resident advocacy groups play a crucial role in ensuring that residents’ rights are upheld. These groups can provide residents with information about their rights, advocate for their needs, and help them resolve disputes with the facility.
- Information and education: Advocacy groups provide residents with information about their rights and responsibilities, as well as about the services and resources available to them.
- Advocacy and support: Advocacy groups advocate for residents’ rights and needs, including by filing complaints with the state licensing agency or by assisting residents in resolving disputes with the facility.
- Training and education: Advocacy groups can provide training and education to staff and residents about resident rights and responsibilities.
Staff Qualifications and Training: Assisted Living Facility Regulations

Ensuring the safety and well-being of residents in assisted living facilities relies heavily on the competence and dedication of the staff. Regulations across various states and regions Artikel specific qualifications and training requirements for staff members, aiming to guarantee a high standard of care.
Minimum Qualifications and Training Requirements
The minimum qualifications and training requirements for staff in assisted living facilities vary significantly depending on the state or region. Generally, most states mandate a combination of education, experience, and training in specific areas related to resident care.
Navigating the complex world of assisted living facility regulations can be as intricate as securing financing for a private jet. Just as you’d want expert legal guidance when making a major aircraft purchase, as outlined in Aircraft Financing Legal Advice A Guide to Navigating the Skies , ensuring compliance with all relevant laws and regulations is crucial for smooth operations and a secure future for your assisted living facility.
- Education: Many states require staff members to possess a high school diploma or equivalent, while some may require a higher level of education, such as a certificate or associate degree in a relevant field, such as gerontology or long-term care.
- Experience: Prior experience in working with seniors or in a healthcare setting is often preferred, and some states may require a specific number of hours of experience.
- Training: Mandatory training is typically required in areas such as:
- First Aid and CPR
- Medication Administration
- Resident Rights and Abuse Prevention
- Infection Control
- Emergency Preparedness
- Safety and Security
- Communication and Interpersonal Skills
Importance of Ongoing Staff Training
Ongoing staff training is crucial to ensure that staff members stay up-to-date on the latest best practices, regulations, and advancements in resident care. It also helps to:
- Improve Resident Care: Ongoing training can enhance staff members’ knowledge and skills in areas such as dementia care, medication management, and assisting residents with activities of daily living.
- Enhance Safety: Training on safety protocols, emergency preparedness, and incident reporting can minimize the risk of accidents and ensure prompt and effective responses in emergencies.
- Promote Compliance: Regular training ensures staff members are aware of and comply with relevant regulations and licensing requirements.
- Boost Staff Morale: Investing in staff training demonstrates a commitment to their professional development, which can improve job satisfaction and retention.
Staff Requirements Across Different States or Regions, Assisted living facility regulations
There are significant variations in staff qualifications and training requirements across different states and regions. Some states, like California, have stricter requirements, demanding more extensive training and experience for staff members. Other states, like Texas, have less stringent requirements.
Assisted living facility regulations are complex and constantly evolving, making it crucial for operators to stay informed and compliant. Navigating these legal intricacies can be challenging, but a knowledgeable business law attorney can provide invaluable guidance. For instance, Business Law Attorney Your Guide to Legal Success can help ensure your facility adheres to all applicable regulations, minimizing the risk of costly fines or legal disputes.
Understanding these regulations is essential for protecting your residents, your business, and your reputation.
- California: The state of California mandates that assisted living facilities have a registered nurse (RN) on staff for a certain number of hours per week. It also requires staff members to complete a comprehensive training program covering a wide range of topics, including dementia care, medication administration, and emergency preparedness.
- Texas: In Texas, the requirements for staff qualifications and training are less stringent. While staff members must complete basic training, the state does not require a specific number of hours or a mandatory RN on staff.
Financial Transparency and Disclosure
Financial transparency and disclosure in assisted living facilities are crucial to ensure resident safety, protect their rights, and maintain public trust. State regulations mandate that these facilities provide residents and their families with comprehensive financial information, promoting accountability and informed decision-making.
Disclosure Requirements
States typically require assisted living facilities to disclose specific financial information to residents and their families. This information helps potential residents make informed choices about their care and understand the financial implications of their decisions.
- Fee Schedule: This Artikels the various fees charged, including monthly rent, service charges, and additional fees for specific services.
- Financial Statements: Facilities are often required to provide audited financial statements, which reveal their overall financial health and management practices.
- Contractual Agreements: These documents detail the terms of residency, including responsibilities, rights, and obligations of both the facility and the resident.
- Policies and Procedures: Information on how resident funds are managed, including policies regarding resident accounts, personal funds, and the use of resident funds for services.
State Agency Oversight
State agencies play a critical role in monitoring the financial practices of assisted living facilities. They ensure compliance with financial transparency regulations and investigate any allegations of financial mismanagement.
Assisted living facility regulations are often complex, balancing the needs of residents with the operational requirements of the facility. Similar to the Airport Operations Law Navigating the Complexities of Air Travel , these regulations aim to ensure a safe and efficient environment, albeit for a different type of passenger. Assisted living facilities, like airports, require careful planning and coordination to ensure the well-being of their occupants and the smooth operation of their services.
- Audits: State agencies conduct regular audits to verify the accuracy of financial records and ensure that facilities are operating within their budgets.
- Investigations: They investigate complaints from residents or their families regarding financial issues, such as improper billing, misuse of resident funds, or lack of transparency.
- Enforcement Actions: If violations are found, state agencies can impose sanctions, such as fines, suspension of licenses, or other corrective actions.
Resident Rights and Protections
Financial transparency is essential for protecting resident rights. By providing access to financial information, residents and their families can:
- Make Informed Decisions: Compare costs and services across different facilities and choose the option that best meets their needs and financial resources.
- Monitor Finances: Ensure that they are being billed accurately and that their funds are being used appropriately.
- Advocate for Themselves: Raise concerns or disputes with the facility and seek resolution through state agencies or other channels.
Complaint Procedures and Enforcement
Assisted living facilities are subject to regulations and oversight to ensure the safety and well-being of residents. This includes robust complaint procedures and enforcement mechanisms to address potential violations and protect residents’ rights.
Procedures for Filing Complaints
Complaints against assisted living facilities can be filed by residents, their families, or other concerned individuals. The process for filing a complaint typically involves contacting the state’s licensing agency or a designated authority. These agencies are responsible for investigating complaints and taking appropriate action.
- Written Complaints: Most states require complaints to be submitted in writing, providing details of the alleged violation, including dates, times, and specific evidence.
- Oral Complaints: Some states may accept oral complaints, but they are usually documented by the agency for record-keeping purposes.
- Anonymous Complaints: While some states allow anonymous complaints, they may be more difficult to investigate due to the lack of identifying information.
Complaint Investigation and Enforcement
Upon receiving a complaint, the licensing agency initiates an investigation to determine the validity of the allegations. The investigation may involve:
- On-site Inspections: Investigators conduct on-site inspections to observe the facility’s operations, review records, and interview residents and staff.
- Review of Records: Investigators examine facility records, such as resident files, incident reports, and staff training records.
- Interviews: Investigators interview residents, staff, and other relevant parties to gather information about the alleged violation.
If the investigation confirms a violation of regulations, the agency takes enforcement action, which may include:
- Issuing Citations: Formal citations are issued to the facility, detailing the specific violations and requiring corrective action.
- Imposing Fines: Financial penalties may be imposed for violations, ranging from minor fines to substantial amounts depending on the severity of the violation.
- Issuing Orders to Correct Violations: The agency may order the facility to take immediate action to address the violation, such as implementing new policies or procedures.
- Imposing Probationary Status: The facility may be placed on probationary status, requiring close monitoring and regular inspections to ensure compliance.
- Suspension or Revocation of License: In cases of serious or repeated violations, the facility’s license may be suspended or revoked, effectively closing the facility.
Emerging Trends and Future Directions
The assisted living sector is undergoing a period of rapid change, driven by evolving demographics, technological advancements, and shifting healthcare paradigms. These trends are shaping the regulatory landscape, prompting policymakers and industry stakeholders to rethink the traditional approach to oversight and quality assurance.
Technological Advancements in Assisted Living
The integration of technology is transforming the way assisted living facilities operate, providing residents with greater independence and enhancing care delivery.
- Telehealth and Remote Monitoring: Telehealth platforms allow residents to connect with healthcare providers remotely, reducing the need for frequent hospital visits and improving access to specialized care. Remote monitoring devices can track vital signs, medication adherence, and activity levels, enabling early intervention and proactive care management.
- Smart Home Technology: Smart home devices, such as voice assistants and automated lighting systems, can enhance residents’ safety, comfort, and independence. These technologies can help residents with tasks such as controlling appliances, receiving reminders, and summoning assistance.
- Robotics and Artificial Intelligence: Robots are being explored for various tasks in assisted living settings, including medication dispensing, meal preparation, and companionship. AI-powered systems can analyze data to predict resident needs, optimize staffing schedules, and personalize care plans.
The ever-evolving landscape of assisted living facility regulations underscores the importance of staying informed. By understanding the regulations, residents, families, and facility operators can work together to create a supportive and enriching environment for seniors who choose assisted living.



